For some people sleeping with Diabetes is one of the scarriest things. What if you go low and don’t wake up? What if you go high and don’t notice it until the morning. For many years I never had problems with sleeping as a diabetic, maybe because I found a system that works well for me. So you might think to yourself “great, she has it all figured out, what about me?“ Don’t worry. I’m here to share my tips and my experience.
Sleeping with Diabetes: Is it really that hard?
Be prepared
No matter if you are on a pump or on injections, you should be prepared for a middle of the night low. There is nothing worse than waking up in the middle of the night, feeling low and having to go on a search for a snack first. Been there, done that. Not one of my fondest memories. So be prepared.
 This is a picture of my nightstand. Besides the usual essentials of a lamp, my glasses, some tissues and my I-Pad I also have snacks on there. I differentiate between mild and bad lows. Mild lows are usually between 3.9 and 4.8 mmol/l (70-86 mg/dl). A bad low is anything below 3.8 mmol/l (68mg/dl). With a mild low 3-4 dextrose tablets are enough to keep me going. Bad lows on the other hand require a bit more attention. So I’ll drink the Ice-Tea and eat some of the corn-waffles. Be sure to choose things, that are easily opened. If you’re just waking up at 3 a.m, are low and don’t know what’s going on you want something fast.
This is a picture of my nightstand. Besides the usual essentials of a lamp, my glasses, some tissues and my I-Pad I also have snacks on there. I differentiate between mild and bad lows. Mild lows are usually between 3.9 and 4.8 mmol/l (70-86 mg/dl). A bad low is anything below 3.8 mmol/l (68mg/dl). With a mild low 3-4 dextrose tablets are enough to keep me going. Bad lows on the other hand require a bit more attention. So I’ll drink the Ice-Tea and eat some of the corn-waffles. Be sure to choose things, that are easily opened. If you’re just waking up at 3 a.m, are low and don’t know what’s going on you want something fast.
Quick Info on why I don’t keep my blood sugar meter on my nightstand: I have a CGM (more about that later in this post) so I don’t need my meter during the night. I had my meter on my nightstand for a while but I kept forgetting to take it with me in the mornings, so for now it just stays in my purse.
No active Insulin at bedtime
Let’s say you had your dinner, bolused for it but had a snack later on with a bolus as well. Don’t go to bed if you still have active insulin on board. Why? If you check your sugar and it’s within range, you could still drop later on if you have active insulin on board. For Pump users: you can see the amount of active insulin on there. Anything below 0.5 Units usually means you’re good to go. For people on injections: try to remember the times where you give yourself insulin. It takes about 2-3 hours for your body to absorb all the insulin. So if you eat and bolus at 7:30 PM and want to go to bed at 9 PM I would wait a bit longer and check my sugars around 10 PM.
If you are anything like me, you like snacks. I mean who doesn’t. If I have a snack after 8:30 PM on a week day I try to eat something without carbs. That way I don’t have to give myself insulin and wait the 2-3 hours for all the active Insulin to be gone. One of my all time favorite snacks are baked almonds. I wrote a whole blog post about them HERE.
Consider getting a CGM, it will bring you so much peace
On average we sleep between 6 and 10 hours each night. This is a long time blood sugar wise where you don’t know what’s going on. To avoid that, consider getting a CGM. It will make sleeping with Diabetes much for peaceful. CGM stands for Continuous Glucose Monitoring. A CGM measures your blood sugars for you. I will do a whole seperate post about CGM and how it works later on. But know this: It’s a Sensor that measures the fluid around you body cells and gives you a glucose reading. This data is transmitted to a device (phone, pump, receiver) where you can see it on a graph. Most CGM Systems will alarm you, if you are low. With the Medtronic Minimed 640g (the pump that I have) it will even alarm you if it senses you going low.
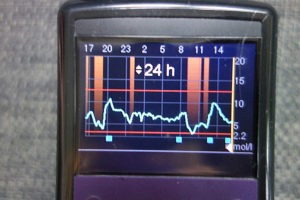
This is a picture of the cgm graph on my pump
Now you may think that you won’t wake up from an alarm from your CGM. Trust me, you will. When I first had my pump I was so irritated with my neighbour because he wouldn’t turn off his alarm on a sunday morning. Turns out it was the alarm from my pump, informing me of a low. I’m one of the deepest sleepers you’ll ever meet. If I’m asleep, I’m asleep and it takes a lot to wake me up. But I hear the Alarms from my pump. They are hard not to hear because they are so loud and obnoxious.
Extra Tip if you already have a CGM: Calibrate right before you go to sleep. That way you can rest for more than 10 hours before you have to calibrate again 🙂
Where to put your pump
To everyone on injections or the Omnipod: I envy you. To everyone else: I feel you. You just wanna fall in to your bed, snuggle up and sleep. But where do you put your pump? I’m a person that never sleeps on their belly so for me the decision was pretty easy: I wear it on the front of my pants. I snapped some pictures for you so you get the idea.


I don’t put it on my hips since I like to sleep on my side. Some nights, if it’s really hot and I only sleep in a shirt, I will just lay my pump next to me and hope for the best. I never had my pump fall out of my bed or something.
Don’t stress yourself out
Waking up from a low in the middle of the night happens to all of us. Even if you follow all the tips you can find and have the best basal for yourself figured out, you might go low during the night. It happens. Try to keep calm and treat your low. Be sure to not overtreat: More carbs won’t bring you up faster, just higher. If you’re living with someone, tell them how they can help you with lows in the middle of the night (if they’re willing to help). This will make sleeping with Diabetes easier since you’re not alone.
I hope this tips help you to get a good night’s rest, making sleeping with diabetes easier. If you have your own tips, share them in the comments. I would love to hear them.